#KidneyWk 2017: Serum and Dialysate Electrolytes and the Risk of Sudden Cardiac Death
One of the last sessions of ASN Kidney Week was “New Methods to Improve Cardiovascular Outcomes in ESRD Clinical Practice” or, in other words, as Tariq Shafi noted, it seemed appropriate to close out out Kidney Week with a session on sudden cardiac death.
Ending #KidneyWk with sudden death
— Tariq Shafi (@DrTariqShafi) November 5, 2017
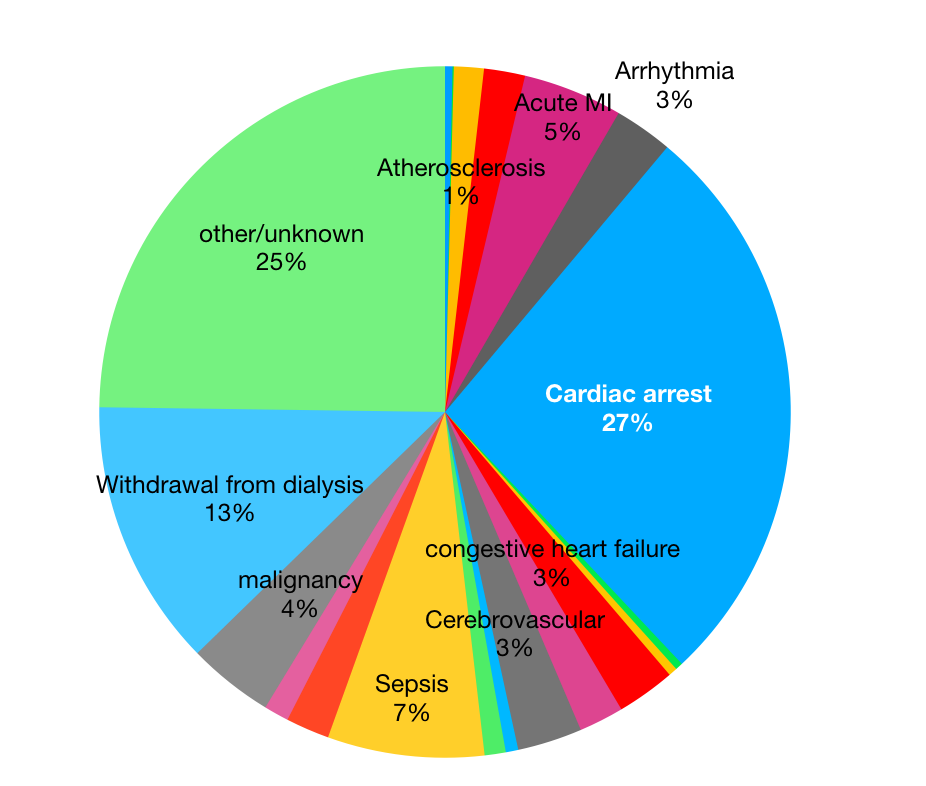
The first speaker was Dr. Patrick Pun from Duke with a lecture titled Arrhythmias and Sudden Death: Role of Dialysate. He started with a pie chart from the USRDS which broke down the various causes of death in dialysis patients. He called it “the infamous pie chart of death.” Grim but true. Cardiac arrest represents roughly a quarter of all deaths.
Then Pun showed Bleyer’s 2006 data that sudden cardiac death does not occur independent of the timing of dialysis but has a bimodal distribution, with peaks within 12 hours of starting dialysis and in the hours preceding dialysis after the two-day break over the week-end (Monday or Tuesday dialysis).
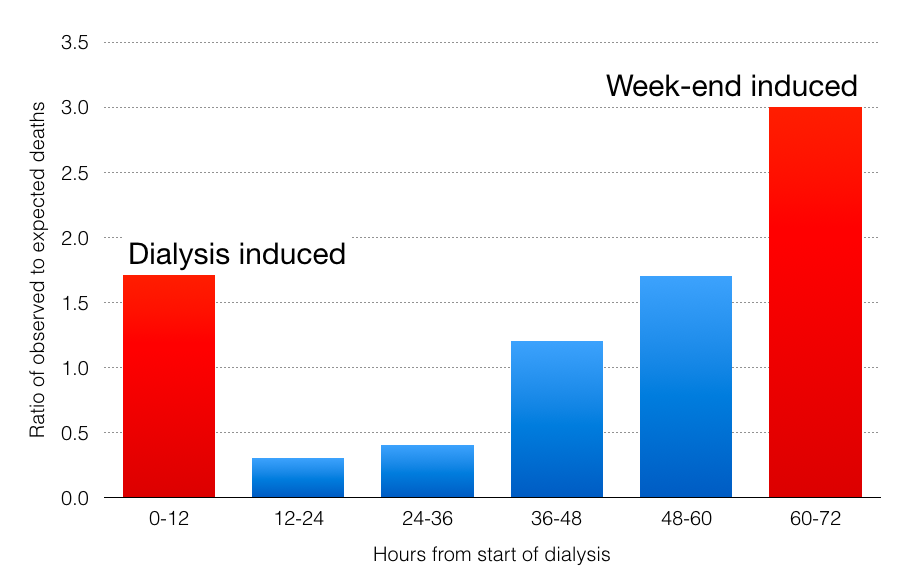
This sparked the theory that there are two factors that are driving sudden cardiac death:
- Accumulation of uremic substances over the prolonged gap from dialysis that happens every weekend.
- Electrolytes or hemodynamic changes that occur during dialysis itself that trigger dialysis.
Using that as his frame, he then did a deep dive on potassium with shallower examinations of calcium and bicarbonate.
Serum Potassium
From Davita’s data, fully 45% of dialysis patients have an abnormal serum potassium pre-dialysis. Incredible.
What are the results of those abnormal potassiums? Pun et al in 2011 showed a U-shape curve for the pre-dialysis potassium for witnessed sudden-cardiac death in the dialysis unit. The lowest risk of arrest was with a pre-dialysis potassium of 5.0. Looking at all-cause mortality, potassium levels has a U-shaped curve with the low point at 4.6 to 4.99. Pun pointed out that the increased mortality with the lower potassium disappeared when the data was adjusted for case mix and malnutrition and inflammation. The mortality at high potassium was less affected by those adjustments.

He closed out serum potassium with DOPPS data showing increased arrhythmia and mortality with pre-dialysis hyperkalemia, but no signal with high-normal potassium.
Dialysate Potassium
Pun then looked at dialysate potassium. He pointed out that dialysate potassium varies tremendously around the world. For example, 2 K baths are used in 43% of patients in Europe, 100% of patients in Japan, and 71% of patients in North America. This variability exists without any significant difference in pre-dialysis serum potassium.
Looking at retrospective analysis, 20% of sudden cardiac deaths occurred in patients on 1 K baths and tragically, the mean pre-dialysis potassium for those patients was an unremarkable 4.9 mmol/L. The excess risk of sudden cardiac death from low potassium baths decreased as the pre-dialysis potassium got higher, but at no point was the low potassium bath actually protective from sudden cardiac death. High potassium baths (over 3) were also dangerous, but 2K and 3K baths were equivalent. One final point on dialysate potassium: it is easy to only look at dialysate potassium, but along with the potassium bath, the bicarbonate also has a profound effect. Higher dialysate bicarbonate leads to a lower potassium during dialysis.
Pun wrapped up potassium by pointing out that there were no randomized controlled trials on potassium and that everything he has shown was retrospective in nature. He did note that in a RCT, fludrocortisone did not lower potassium in dialysis patients; however, bisacodyl did. Kayexalate works but has limited patient adherence. The newer potassium binding agents look promising but still lack large-scale studies to back that up. He noted that matching dialysate potassium to serum potassium holds promise and that employing the dialysis dieticians makes sense for this. He pointed to the experience of Lee and Mendelsohn who had success with this.
After this Pun went on to discuss calcium and bicarbonate. Unfortunately, this was less nuanced and more rushed as he tried to get done before the orchestra started playing and they hooked him off the stage. He started with data showing that as the calcium falls during dialysis, the QTc rises.
Pun did a matched case control study of 2,100 patients and found a 50% increase in risk of sudden cardiac death with a dialysate calcium below 2.5 mEq/L. He also found that the risk rises as the gradient between serum calcium and dialysate calcium rises. He pointed out that things are not simple and we need to be aware of interactions between electrolytes. He showed data from Genovesi et al demonstrating that the prolonged QTc of low dialysate calcium is ameliorated by higher potassium baths (3K had shorter QTc than 2K baths). He finished the calcium section by emphasizing that sudden cardiac death is only one of multiple outcomes affected by dialysate calcium and that avoiding SCD may conflict with other goals like avoiding vascular calcification. Studies in this area will need to look at the full breadth of outcomes rather than just focusing on QTc or arrhythmia.
The last bit that Pun examined was bicarbonate. He only had a few slides here. The first slide looked at the relationship with serum bicarbonate and mortality. Here there is a well documented association with increased bicarbonate and increased risk of death. The interesting part is that when you add case-mix adjusted risk the association develops the familiar U-shape and if you adjust for both case-mix and malnutrition and inflammation the original curve reverses and most of the excess risk is seen at low bicarbonate.

When looking at dialysate bicarbonate, DOPPS has found an association between higher bicarbonate concentration and increased mortality (HR 1.1) and hospitalizations (HR 1.1). Mortality was driven by increased infections (HR of 1.4), while hospitalizations was driven largely by cardiovascular causes (HR 1.1).
In the question section I asked why, if dialysis is 50 years old, some of these fundamental questions about the fundamental ingredients in dialysate have not been answered in a rigorous way? We have over half a million dialysis patients getting dialysis every week, and it is long overdue to figure these out in a rigorous and prospective manner. No more treating people using rearview mirror research.
.@kidney_boy: why don’t we have RCTs on dialysate composition? pic.twitter.com/KOB10m8lk8
— Nathaniel Reisinger (@nephrothaniel) November 5, 2017
Twitter responded with two questions to be answered with RCT in dialysis patients:
Large pragmatic trial on dialysate Na ongoing @georgeinstitute
— Rajnish Mehrotra (@rajmehrotra1122) November 5, 2017
And
Also on dialysate temp https://t.co/Hp4lzicMMq #KidneyWk
— Swapnil Hiremath @hswapnil@bsky.social (@hswapnil) November 5, 2017
Dr. Pun later gave me an additional answer.
I think RCTs now made possible by new tools including implantable loop monitors and wearable patches to use as proof of concept. Stay tuned
— Patrick Pun, MD MHS FASN (@virtualpun) November 5, 2017
Dr. Pun did a cracking job at wrapping up Kidney week with a great examination of some of the electrolyte abnormalities that may be harming our dialysis patients. I look forward to this talk next year with (hopefully) some more rigorous, and prospective data.
– Post prepared by Joel Topf, AJKD Social Media Advisory Board member. Follow him @kidney_boy.
Don’t forget to check out more AJKDBlog coverage of Kidney Week 2017!

Leave a Reply